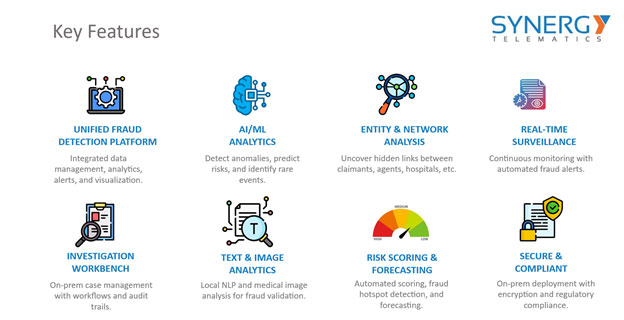
abcHealth delivers an advanced fraud detection platform tailored for insurance firms, combining intelligent data integration, analytics, and visualization into one unified system. Powered by AI and machine learning, it helps insurers detect anomalies, assess risk, and uncover rare fraud events with precision. The platform provides deep entity and network analysis to reveal hidden relationships between claimants, agents, providers, and other actors. Real-time surveillance ensures continuous monitoring and instant fraud alerts, while the investigation workbench supports efficient case management with full audit trails. With built-in text and image analytics, insurers can validate claims using local NLP and medical image data. Automated risk scoring and forecasting enable proactive fraud prevention and hotspot detection. Fully secure and compliant, Synergy’s solution supports on-premise deployment with encryption and regulatory alignment, giving insurers confidence and control over their fraud operations.